Accurate Prediction of Vancomycin Levels to Optimize Care
In this article:
DoseMeRx Leverages Pharmacometrics for Dose Optimization of Vancomycin
DoseMeRx is unique precision dosing software that incorporates clinically validated pharmacokinetic drug models, patient characteristics, drug concentrations and genotype (if applicable and available) to guide dose optimization.
Designed exclusively to support physicians in making a rigorous, best-practice decision based on maximizing the use of readily available patient data via pathology and other sources.

Individualize doses to any therapeutic target

Custom physiciandriven dosing

Hospital Guidelines

Drug label dosing
Indvidualized dose recommendations in target trough range
Reduction in supra-therapeutic troughs

Make use of every vancomycin concentration, including those outside of the recommended time predose
How Accurate is DoseMeRx at Predicting a Concentration?
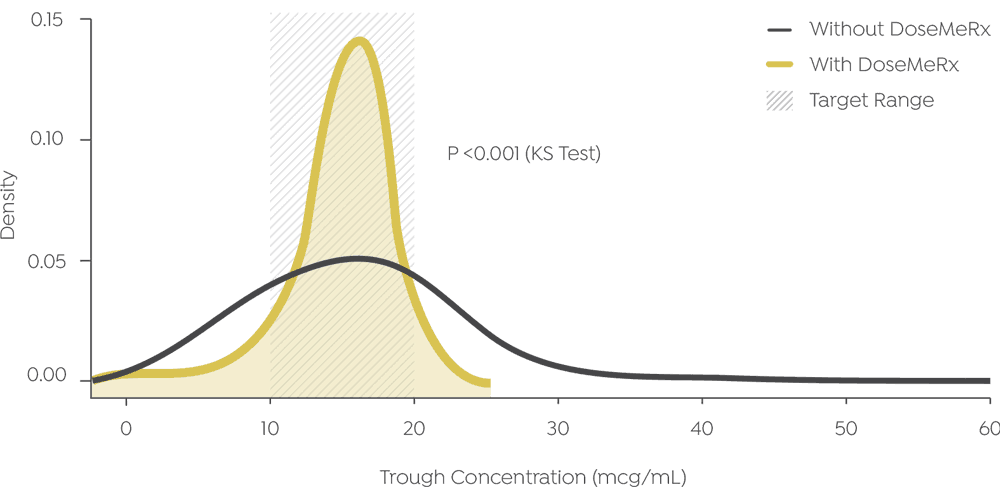
DoseMeRx can accurately predict the concentration of vancomycin levels with low error relative to the target trough range (10-20mcg/mL):
Mean Error: 1.2mcg/mL
Mean Absolute Error: 2.9mcg/mL
DoseMeRx maximizes
the use of every
vancomycin
concentration, even
those outside of the
recommended time
pre-dose.
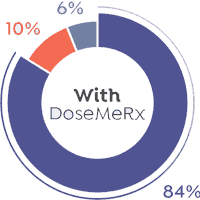
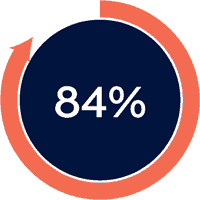
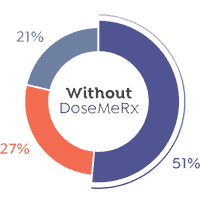
DoseMeRx can place 84% of doses into the target range, and is significantly less likely to result in overexposure, reducing patients at risk of acute kidney injury from 27% to 10% of doses.
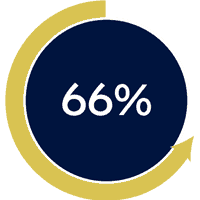
Without DoseMeRx, only 1 in 2 doses achieved troughs considered therapeutic by the AME guidelines1. Why is this proportion so low?
- Only 14% of vancomycin levels were taken within AME guidelines of within 30 minutes prior to a dose. The mean time that a level was taken prior to the next dose was 320 minutes (5.3 hours). Without model-informed dosing, such as DoseMeRx, these levels are largely useless.
- Vancomycin has high inter-individual variability. Studies show that the vancomycin dose-effect relationship is sufficiently variable that a population of patients receiving 1000mg bd can have trough levels ranging from 5.3–72.6mcg/mL2
Reduce the risk of vancomycin nephrotoxicity with DoseMeRx
Nephrotoxicity is a major concern for vancomycin
dosing, and a significant adverse event 3.
The literature supports precision dosing using
decision support software like DoseMeRx as an
effective approach to optimizing vancomycin dosing 4.
DoseMeRx consistently and more accurately can calculate a dose to place a patient in the therapeutic range. The accuracy of DoseMeRx allows physicians to significantly decrease the proportion of vancomycin doses with supra-therapeutic troughs from 3/10 to 1/10.
The proportion
of patients at risk for
vancomycin-induced
nephrotoxicity risk
can be significantly
reduced with
precision dosing.
Vancomycin Dosing and Monitoring
Vancomycin has a narrow therapeutic range, with clinical practice targeting a therapeutic trough of 15-20mcg/mL. Toxicity of vancomycin is exposure-dependent, with high trough concentrations shown to significantly increase risk of nephrotoxicity5,6. Accurately reaching therapeutic targets is critical to effective treatment and minimization of antimicrobial resistance7.
DoseMeRx allows
calculation of
both trough
or AUC24.
The Evaluation
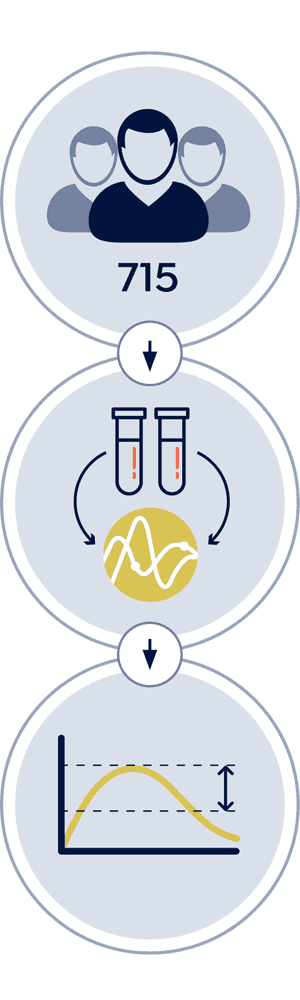
Data
- 715 patients receiving vancomycin
- Dosed prior to DoseMeRx introduction at two large
teaching hospitals - Physicians targeted troughs of 10-20mcg/mL
Method
- We selected 57 courses with multiple assay levels
- Data was input into DoseMeRx, excluding the final blood level
- We measured how accurately DoseMeRx predicted each
withheld assay result
Outcomes Measured
- DoseMeRx’s accuracy and bias of predicting the
next assay level - Proportional accuracy to determine how often DoseMeRx calculates a dose precisely enough to place patients in the therapeutic range
Try DoseMeRx – Free Trial
Try DoseMeRx for yourself, with a free 14 day trial including your choice of drug packages from a wide range of medications, customize dose or target functions to individualize treatment for every patient, and access our mobile and tablet apps for iOS and Android. During your free trial, you’ll also have access to our support team who are here to answer any questions you have. Start free trial now >>
References
- Rybak MJ et al. Pharmacotherapy. 2009 Nov;29(11):1275-9.
- Neely MN et al. Antimicrob Agents Chemother. 2014;58(1):309-16
- Filippone EJ, et al. Clin Pharmacol Ther. 2017 May 5. doi: 10.1002/cpt.726
- Pea F et al. Int J Antimicrob Agents. 2002 Nov;20(5):326-32.
- Bosso JA et al. Antimicrob Agents Chemother. 2011 Dec;55(12):5475-9. doi: 10.1128/AAC.00168-11.
- Suzuki Y et al. Chemotherapy. 2012; 58(4):308-12.
- Ye, Zhi-Kang et al. “ PLoS ONE9.6 (2014): e99044.
